Prior authorization was designed as a cost-control measure, but in practice, it has become a significant barrier to timely cancer treatment. A recent survey by the American Society for Radiation Oncology (ASTRO) revealed an alarming reality.
ASTRO Survey Results:
- 92% of radiation oncologists report that prior authorization causes treatment delays for their patients.
- 35% of patients, on average, experience delays in their treatment due to these requirements.
- 68% of doctors say these delays last five days or more, a sharp increase from 52% in ASTRO’s 2020 survey.
- 33% of oncologists report that this has led to patients abandoning radiation treatment altogether.
- 82% of doctors have been forced to resort to less optimal treatments due to prior authorization barriers.
- Many oncologists struggle to obtain insurance approval for essential medications, with 40% reporting issues with opiate pain medications, 23% for nausea medications, and 10% for non-opiate pain medications.
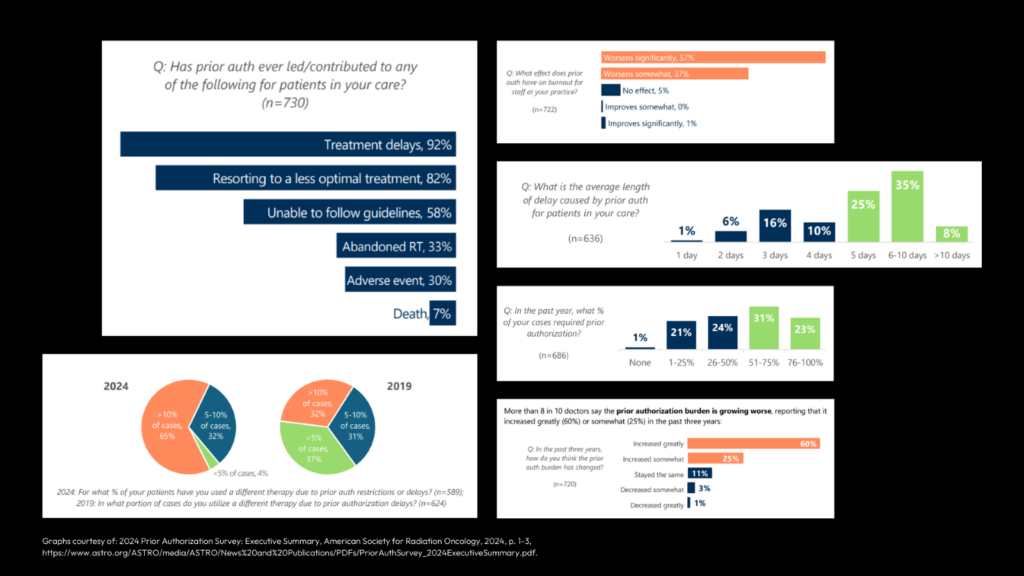
These statistics are more than numbers—they represent real people whose lives are at stake. For cancer patients, every moment counts. Delays in treatment can mean the difference between a successful outcome and a devastating progression of disease. Prior authorization requirements create unnecessary hurdles that slow down care, increase stress for patients and providers, and ultimately compromise health outcomes. This is unacceptable.
Addressing Prior Authorization Challenges with RO Dynamics
Prior authorization remains a major obstacle in delivering timely cancer treatment, but technology can help alleviate these burdens. RO Dynamics streamlines the process through workflow automation, data integration, and real-time tracking, reducing administrative delays that stand between patients and the care they need.
- By automating prior authorization tracking, RO Dynamics helps clinics:
- Reduce delays by keeping the process moving without manual intervention.
- Improve efficiency through seamless integration with EHRs and adherence to FHIR standards.
- Refocus on patient care, ensuring providers spend more time treating patients rather than navigating paperwork.
Breaking Down Barriers to Timely Care
It’s time to eliminate unnecessary delays and put patients first. By leveraging smart automation and interoperability, we can ensure that cancer patients receive the care they need when they need it—not days, weeks, or months later.
Learn more about how RO Dynamics can help streamline prior authorization: Quantek Systems – Optimizing Insurance Prior Authorization
Read the ASTRO report on prior authorization delays: ASTRO News Release
Contact your representatives and urge them to support the Improving Seniors’ Timely Access to Care Act of 2024 to ensure patients receive the care they need without unnecessary delays. Find your representatives here: https://www.congress.gov/members/find-your-member
