Insurance prior authorization is often a complex and time-consuming process that can create bottlenecks in patient care. How can healthcare providers ensure that patients do not fall through the cracks during this critical phase?
At Quantek Systems, our customers have successfully optimized their prior authorization workflows by implementing customized tracking of their patients through this phase, utilizing RO Dynamics to streamline communication. With the help of RO Dynamics, radiation oncology departments are able to manage every step of the process, from the initial draft and submission to appeals and final approvals, ensuring a seamless experience for both patients and providers.
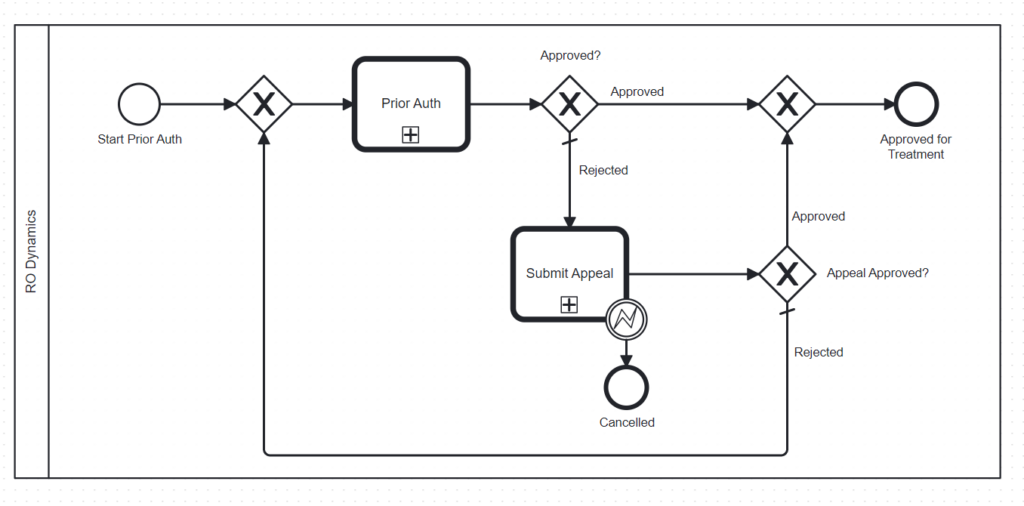
Leveraging BPMN for Workflow Efficiency
RO Dynamics, leveraging Business Process Model and Notation (BPMN), streamlines the insurance prior authorization workflow from the moment a patient is scheduled for simulation in the radiation oncology department. By initiating this process early, financial navigators can help minimize delays that could otherwise postpone a patient’s treatment start date. This proactive approach is key to ensuring timely care and improved patient outcomes, and is feasible for clinics with large patient loads with the help of RO Dynamics.
Seamless Integration with OIS through FHIR
Our integration with the Oncology Information System (OIS) through Fast Healthcare Interoperability Resources (FHIR) enables RO Dynamics to track patients from the moment they are scheduled for simulation. Once the patient is in the system, a BPMN workflow is automatically triggered, notifying the financial navigation team that it is time to begin the prior authorization process. This early notification allows financial navigators to track the status of each patient throughout the process, ensuring no steps are missed.
Enhanced Team Coordination and Communication
The system not only tracks patient progress but also facilitates coordination among team members. Financial navigators can collaborate with other departments to create comparison plans, submit appeal letters when necessary, and arrange peer-to-peer reviews to expedite approvals. This level of coordination reduces the administrative burden and accelerates decision-making.
Adapting to Denials with Alternative Treatment Plans
In cases where a treatment is denied (e.g., proton therapy), the care team can quickly assess and initiate an alternative treatment plan (e.g., photon therapy). This agility prevents unnecessary delays and ensures patients remain on schedule for their radiation oncology treatment. By fostering better communication and workflow efficiency, RO Dynamics helps healthcare providers deliver timely, effective care.
Delivering Timely Care
In summary, RO Dynamics by Quantek Systems offers a robust solution to the challenges of insurance prior authorization. Through early workflow initiation, comprehensive tracking, and enhanced team coordination, we help ensure that patients receive the care they need without unnecessary delays.
Contact us today for a demo or more information and follow us on LinkedIn for the latest news and updates!
